MD Program ForWard Curriculum
Overview
The ForWard Curriculum replaces the traditional model of medical education — two years of basic science followed by two years of clinical experiences — with a three-phase model that fully integrates basic, public health and clinical sciences throughout our medical students’ education. This curriculum lets students engage with clinical learning experiences earlier in their medical school careers. This early entrance into clinical clerkships helps facilitate career exploration and gives UWSMPH competitive edges for residency selection.
Phase 1 (Pre-Clinical) Education Opportunities in the Department of Surgery
SMPH Shapiro Summer Research Program
The UW Department of Surgery has a long tradition in educating medical students in the clinical and the research environments and has been an active participant in the UW SMPH Shapiro Summer Research Program since 2002. Summer research programs in the Department of Surgery aim to provide students with an appreciation for the nature of scientific research. The program includes seminars and additional training opportunities to help develop skills in data collection, analysis, and presentation of results to the medical community. Projects offered are across a diverse field of surgical specialties and may include laboratory-based basic science, clinical research, translational research, health services, and global/public health-related research.
This is an accordion element with a series of buttons that open and close related content panels.
T35 Surgery Summer Research Experience for Medical Students
We offer short-term summer research experiences for medical students interested in research related to diabetes, obesity, endocrine disorders, nutritional disorders, digestive diseases, liver disease, kidney disease, and urologic disease. Funded by a T35 grant from the National Institute of Diabetes and Digestive and Kidney Diseases, the program offers eight students a mentored 10-12 week research and training experience with the goal of encouraging medical students to pursue academic medical careers. The program includes completion of a mentored research project, along with a curriculum designed to teach medical students the essentials of effective research and academic research principles. At the completion of their experience, students write an abstract and present a poster or oral presentation.
Additional information here >>
| Student | Date | Mentor | Topic | Outcomes |
|---|---|---|---|---|
| Chen, Kallie | Summer 2019 | Schenider, David, MD, MS | Thyroid Imaging Reporting and Data System: The Utility of Natural Language Processing Output in Risk Stratification and Reporting Measures | Presentation at Wisconsin Surgical and Academic Surgical Congress |
| Rust, Clayton | Summer 2019 | Gibson, Angela, MD, PhD | Evaluation with cell viability with common wound cleansing agents in ex vivo human skin model | Presentation at Wisconsin Surgical and Academic Surgical Congress |
| Schreiter, Nicholas | Summer 2019 | Weber, Sharon, MD | Etiology of Transitional Care Issue | Presentation at Academic Surgical Congress |
| Schulz, Kathryn | Summer 2019 | Schwarze, Gretchen, MD, MPP | Redesigning Preoperative Conversations | Presentation at Wisconsin Surgical |
| Skelton, Paul | Summer 2019 | Lawson, Elise, MD, MSHS | Decreasing use of opioids for patients undergoing colorectal surgical procedures | Presentation at Wisconsin Surgical and Academic Surgical Congress |
| Mustafa, Ana | Summer 2019 | Al-Adra, David, MD, PhD | Enhancement through Evasion: Liver Transplantation and the Augmentation of pd-L1 | Poster Presentation at the Keck Graduate Institute |
| Warden, Aleah | Summer 2019 | Richards, Kyle | Opioid Use After Urologic Surgery | Poster Presentation at the Keck Graduate Institute |
Voice Research Training Program (T32) for medical students
The Department of Surgery, as well as the UW School of Medicine and Public Health, have well established programs that provide research opportunities for medical students in the summer following their first year of medical school. Using these programs as a platform, this training program will provide short-term summer research opportunities in the field of voice research. The program requires a 10-12 week experience at UW, but the nature of the program requires students to show initiative in preparation for the summer research experience, as well as follow-up work upon completion of the short-term project. Trainees will engage in mentored research project, medical student specific research curriculum, as well as voice research specific conferences and lab meetings to enhance the experience.
| Trainee | Date | Mentor | Project | Outcomes |
|---|---|---|---|---|
| Figueroa, Joanie | Summer 2018 | Connor, Nadine, PhD | Qualification of Lingual Muscle Plasticity | Publication in process |
| Mechler-Hixon, Alexandra | Summer 2018 | Thibeault, Susan, PhD, CCC-SLP | Characterization of toll-like receptors in human vocal fold tissue, murine vocal fold tissue, and human epithelial cells | Presentation at Academic Surgical Congress in 2019 |
| Bach, Kathy | Summer 2019 | Francis, David, MD, MS | Quality of Life Impact of Vocal Fold Paralysis from Thyroid Surgery | |
| Kubica, Phillip | Summer 2019 | Glazer, Tiffany, MD, Additional Mentors: Hartig, Gregory, MD; Francis, David, MD | Outcome of T3/T4 Oral Cavity Squamous Cell Carcinoma Based on Delays from Diagnosis and Treatment |
Surgery Interest Group
This past year the Surgery Interest Group has continued to offer opportunities for M1 students to explore the surgical career field through shadowing opportunities, educational discussion panels, suturing skills labs, and networking events.
The Surgery Interest Group hopes to facilitate relationships and experiences with our department faculty for students interested in pursuing surgery as a career.
Thank you to our SIG Leadership Team for a successful year – even with a pandemic – and to members of our department that contribute to the ongoing success of SIG and efforts to recruit medical students into surgery!
We look forward to expanding the group across phases and promote peer mentorship opportunities for advanced students to assist with incoming students and undergraduate organizations.
This is an accordion element with a series of buttons that open and close related content panels.
2020 Surgery Interest Group Leaders
Medical Student Leaders

“I applied to be a SIG leader because I knew the role would present a great opportunity to learn more about surgery, meet classmates of similar interests, and connect with and learn from physicians who are successful in the field that I am so interested in. I am drawn to surgery because it is a field in which you solve a problem you can see and watch your intervention take form before your eyes, and I have always had a particular interest in plastic and reconstructive surgery.”
-Kasey Leigh Wood, M1
“I’m drawn to surgery for various reasons, but a big one is because of the way it allows for greatly improving a patient’s quality of life in a relatively short amount of time. When working as a research assistant for an orthopedic surgeon who performed hip/knee arthroplasty prior to medical school, seeing the huge shift in quality of life that patients experienced after surgery was incredibly satisfying. A significant number of patients that I worked with went from struggling to walk before surgery to returning to an active lifestyle after surgery, which was amazing to see. Additionally, as a former collegiate athlete, the team aspect of the OR and goal-oriented nature of surgery also appeals to me.
I am certainly not set on any particular specialty, but general surgery (because of the breadth of the skillset and the variety of potential subspecialties) and orthopedics (because of my prior experiences as an RA) both interest me at the moment.
As a SIG leader, I hope to bring consideration of the field of surgery to fellow medical students, particularly those who may not have previously thought about surgery as a possibility. Prior to shadowing in the OR and working with a surgeon during my gap year before medical school, the possibility of becoming a surgeon was not at all on my radar. I think that many medical students have preconceived ideas of what being a surgeon entails and the type of person who becomes a surgeon. Whether a student starts off medical school being entirely set on becoming a surgeon or entirely against it, it’s important to actually get exposure to the field and meet surgeons to learn about who they are and what they do. I think SIG plays an important role in introducing medical students early on in their education to surgery, and giving them resources to help inform them about whether a surgical specialty is something they may be interested in pursuing.”
-Natalie Schudrowitz, M1
SIG Program Director

Assistant Professor
Department of Surgery
Division of Vascular Surgery
Administrators

cookd@surgery.wisc.edu
2019-2020 Events
In August, we welcomed a new cohort of M1 students to campus and to the Surgery Interest Group. Dorothy Cook led an orientation and OR training session to 75 students – giving them clearance to pursue OR shadowing opportunities and what to expect as members of SIG in the coming year.
 In September, Girma Tefera, MD, and Kristin Long, MD, MPH, co-led the Medical Student Surgery Interest Group’s (SIG) first event of the year. Eighty-four first and second year medical students attended the global surgery lunch talk.
In September, Girma Tefera, MD, and Kristin Long, MD, MPH, co-led the Medical Student Surgery Interest Group’s (SIG) first event of the year. Eighty-four first and second year medical students attended the global surgery lunch talk.
In November, the Department hosted the annual faculty/student mixer with the Surgery Interest Group at the Great Dane.  Over 90 medical students, faculty, and residents attended. The event offered the opportunity for pre-clinical students interested in surgery to connect with faculty in a casual setting.
Over 90 medical students, faculty, and residents attended. The event offered the opportunity for pre-clinical students interested in surgery to connect with faculty in a casual setting.
SIG Virtual Events During COVID-19
While the SIG leadership team had several events and opportunities planned for members of the group, the pandemic swiftly called for cancellations – and some creativity.
M4 Panel
In April 2020, the Surgery Interest Group held a virtual panel of M4s who matched into surgical residencies via Zoom.
Attendees were able to learn from the following panel of students:
- 2 medical students who have matched into general surgery
- 1 who has matched into ENT
- 1 who has matched into neurosurgery
- 1 who has matched into orthopedic surgery
- 1 who has matched into urology
This panel represented a variety of subspecialties – and attendees felt that the discussion was informative and helpful – and casually fun!
Surgical Lifestyles Panel
In May 2020, Drs. Dawn Elfenbein, Kristin Long, Ben Zarzaur, and Stephanie Savage led a virtual “Surgical Lifestyles” event for the members of SIG via Zoom.
Over 20 students joined in to hear first-hand how to balance the demands of both work and personal lives in a surgical specialty.
M1 SIG Leaders Natalie and Kasey moderated the discussion with topics of interest submitted by their peers including:
- How do surgeons balance the demands of surgery (e.g. long hours) with family life and/or outside interests?
- What are some of the challenges encountered in finding this balance?
- For surgeons who decided to have children, how did they decide when the right time to have children was?
- Advice for medical students who are considering pursuing a surgical specialty
SIG Fall Events
When the Surgery Interest Group returns in the Fall, we are looking to incorporate some new events, as well as hoping to bring back successful events from previous years that have been sponsored by our department as able.
After surveying interests on proposed events to our group members – we anticipate 60+ students to participate in the following future events – dates TBD:
Research Talk – An event focusing on research in surgical specialties and how to get involved with projects
Pre-SPC Phase II – An event prior to starting Phase 2 on expectations and tips to succeed for the Surgical and Procedural Care (SPC) block
Networking Dinner – A dinner networking event to meet surgical faculty and residents in various specialties
Suture Skills as able…
Phase II Integrated Clinical Blocks
12 Months | January – December
Surgical and Procedural Care Block
Overview
In Phase II students are exposed to clinical learning experiences for the first time. The Department of Surgery hosts four blocks of students every year in this phase for their Surgical and Procedural Care requirement. In SPC students are exposed to clinic-based learning and exposed to services that collaborate on the management and care of surgical patients.
In addition to their scheduled service rotations, students are assigned a continuity clinic preceptor that they longitudinally follow through their entire 12-week block on SPC. This opportunity gives students a chance to spend additional time in a service they are interested in and gain a stronger relationship with a faculty member.
This is an accordion element with a series of buttons that open and close related content panels.
Phase 2 SPC Leadership

Integrated Block Lead

Block Co-Lead

Block Co-Lead

Education Coordinator (Surgery)

Phase II Coordinator (MEO)
Thank you to the following faculty for serving as educational leaders within your divisions and for your contributions to our medical student education in both Phase II and III:
General Surgery
Blue Team- Sean Ronnekleiv-Kelly
Gold Team – Amber Shada
Green Team – Lee Faucher
Orange Team – Chip Foley
Pediatric Team – Adam Brinkan
Red Team – David Melnick
VAH Team – Christina Geltzeiler
Cardiac – Amy Fiedler
Thoracic – Daniel McCarthy
Otolaryngology – Greg Hartig
Plastics – Venkat Rao – *now Del Mount
Transplant – Robert Redfield
Vascular – Paul DiMusto
Anesthesia – Karin Zuegge
Interventional Radiology – Mark Kleedehn
Neurosurgery – Nathaniel Brooks
Ophthalmology – Dan Knoch
Urology – Tracy Downs
Curriculum Updates
This past year, we implemented new initiatives and curriculum developments for students rotating within our department, and across our statewide campuses, during the Surgical and Procedural Care Block.
This is an accordion element with a series of buttons that open and close related content panels.
Longitudinal Patient Project - Updates
Background Information on the project goals for students:
Relying on experiential and reflective learning – this project was designed as a self-directed assignment that is intended to give students an opportunity to assemble a unique, comprehensive, and team-based integrative care experience in an effort to gain a more comprehensive picture of caring for surgical patients. Students will have the opportunity to learn through the experience of identifying a patient in clinic, following the patient from Pre-Operative to Post-Operative care, and reflection and critically analysis of the internal and external mechanisms that impact patient care.
Objectives of the project are outlined below:
- To assemble a unique and integrative care experience through self-direction and collaboration with members of the care team to gain a more comprehensive understanding of caring for surgical patients.
- To recognize the importance of interprofessional relationships and collaboration in caring for patients by understanding and respecting the roles of healthcare providers involved in surgical patient care.
- To recognize the influence that comorbidities have on surgical care plans through critical analysis of the risks and decisions to proceed/not proceed on operation.
- To apply theory into practice through the synthesis of evidence-based medical literature and their experience in an effort to discuss and solve problems and stay current and progressive with advancements in healthcare.
- To recognize socioeconomic disparities that exist in healthcare and the barriers that these place on the decisions made to seek treatment and towards creating a sustainable healthy environment
Pilot to Full-Scale Learning Opportunity
After moving from the successful pilot stage of the Longitudinal Patient Project, the assignment was disseminated to all students in SPC in Madison and statewide:
Tech Advantages
The SPC team was able to overcome logistical and scheduling barriers to assist with achieving the goals of this project and offering this experience to our students with the help and collaboration of our IT Development Team Members – Steve Van Der Weide, Sean McMullin, and Richard Nelson. The dev team rose to the occasion to create a personalized application within our intranet for students to schedule patients to follow to complete their project securely and within HIPAA compliance guidelines.
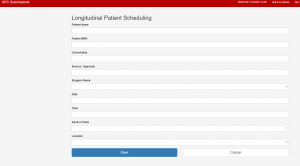 The application was well received and user friendly for students and administration to track student progress on the assignment and to ensure students were included in communications to all team members participating in the operation.
The application was well received and user friendly for students and administration to track student progress on the assignment and to ensure students were included in communications to all team members participating in the operation.
Students and administrators would receive application/e-mail notifications on the status of their submission – denied, pending, approved, scheduled, based on the student’s submission content and compliance with project guidelines.. This application was a much needed tool for the success of this project and we are so grateful to have the innovative IT team to help move or education initiatives forward.
Expansion Opportunities – Fewer Restrictions for Students
Special thanks to our partners in Anesthesia for being outstanding collaborators and leaders on this venture – and for facilitating partnerships with our hospital network to remove restrictions and promote opportunities for students to participate in this project at all of our locations – including TAC, VAH and Meriter – additional thanks for Dr. David Melnick for being a key player and advocate for his students and for acting as a catalyst to include Meriter as a location for this project.
Mid-Rotation Discussion Forum
Promoting Positive Experiences and Communication through Peer-Focused, Synchronous, Discussion Forums
Objective
To foster a peer-to-peer teaching and learning environment to enhance student experiences in the surgical clerkship.
Overview
Within the 12-week surgical clerkship (Surgical and Procedural Care), a forum of medical student peers and research residents were organized at the midway point to meet with the current cohort of SPC students. The development of this forum was intended to promote better learning experiences for students rotating in their surgical clerkship by fostering a peer-to-peer teaching and learning environment.
This session provides students an opportunity to touch base with peers that have successfully completed the surgical rotation and residents currently in their research years, as an opportunity to ask questions and learn strategies to apply into the remainder of their block to promote a better learning experience. This was developed in response to negative feedback and mistreatment concerns that often arise in surgical rotations.
Implementation Goals
For the Novice Learners
- Provide an opportunity for active learning through interactions between students
- To strengthen confidence in their abilities to do well on their rotations
- To facilitate a comfortable learning environment that students were able to ask questions to improve their learning environment and apply what was learned into practice for the remainder of their time on SPC
- To provide students with psychological benefits, such as cathartic release and sense of community
For the advanced learners/facilitators
- Increase confidence in their own ability to teach and seeing r growth since being in the Phase II learners roles
- Consolidate learning and strengthen own knowledge and skills (both in context and as teachers)
- Develop communication skills and use impactful communication to listen, provide direction, and adjust the course of the discussion to meet the needs of the students to set them up for success
- Assess Learning and strengthen their ability to assess the students understanding and provide clarity
Planning and Evaluation of the Forum
Planning
This session required recruiting a diverse student/resident panel and scheduling of the session by aligning with the current didactic schedule.
Evaluation
Following our first few sessions, the feedback from the learners and facilitators was inspiring. Students reported that this session provided many benefits such as a sense of community, comfortable learning environment, was cathartic, and beneficial.
The advanced learners felt that they gained new beneficial perspectives as learners and teachers.
This session will be evaluated for its effectiveness through a self-reporting survey of attendees and by measuring student feedback trends going forward.
Special thanks to Aos Karim, PhD and Sarah Jung, PhD for being co-leads on the successful implementation of this meaningful opportunity.
Unanticipated Outcomes - Integration into SPC
Building off of the work of Dr. Jamie Hess and Amy Becker, we successfully adopted the Unanticipated Outcomes exercise and offered this to students rotating in SPC. As we piloted this session into our course, we opted to create an opportunity that our statewide sites could also participate in – which we successfully offered in February 2020 and served as a timely introduction to telehealth for our students.
During this exercise, our Phase 2 medical students participate in 2 standardized patient encounters in which they will deliver news regarding an error to a patient or family member via telehealth.
Each student will participate as the Acting MD in one of the two cases, and swap and observe their peers participation in the other case.
Since SPC has taken the Unanticipated Outcomes DTA into the course, we have planned to offer this to the remaining Phase II students who have yet to complete SPC within the “interim course.” We piloted this session in a virtual format in Block 1 of 2020 to offer to our away site students – which for once has given us the benefit of being ahead of the curve and we look forward to integrating this session into the online curriculum.
Students were able to learn through experience and observation during this exercise and receive meaningful feedback from the SP’s, their peers, and faculty facilitators and we look forward to facilitating this meaningful opportunity using an entirely online platform..
Synchronous & Asynchronous Radiology Lectures
A new collaboration with our radiology colleagues gives our students an opportunity to learn the basic anatomy and key features for respective diagnosis and to better prepare our students to work through our neuro, abdominal, and head and neck case discussions and to be applied into their clinical practices.
This course uses a web-based DICOM/PACS viewer to look at real radiology studies, which will help students to learn the essentials of imaging viewing and make connections between gross/radiologic anatomy and start to familiarize themselves with imaging of surgical diagnoses. The ability to pull up a radiology study, scroll through the images, and find the relevant anatomy are key but often overlooked skills, so take time to build a strong foundation.
In this course, students are given the opportunity to become more familiar with working with and manipulating radiology images, review key normal anatomy interactively, and practice this through cases.
This session was piloted in 2019 in-person as three separate one-hour lectures, but are now available as an online asynchronous modules – please see the links below to review this content.
Special thanks to Tabassum Kenedy, Michael Hartung, and Jason Stephenson in the Radiology Department, as well as Katie Yang.
SPC "Hall Pass"
This January, our SPC leadership team created an opportunity for our medical students to have additional autonomy and drive over their own education. Acknowledging the fact that often educational benefits that arise on service may interfere with other SPC block expectations, and that students may need to miss out on a meaningful opportunity, we created an alternative learning assignment, now known as the “Hall Pass”.
This opportunity was implemented to promote autonomy and self-directed learning for our students, in the instance they are presented with a unique learning opportunity that may conflict with a requirement of SPC – i.e a scheduled Case Discussions or Continuity Clinic.
In these circumstances, students and faculty can decide whether the opportunity presented offers more educational benefit than attending CBL or CC without administrative approval. Students are required to complete the “Hall Pass” slip and have this signed by the faculty member who is supervising the student in the alternate learning activity.
Since being integrated into SPC for a few months, two students have already used the hall pass. One of the students used this to participate in an incredibly unique and rare procedure. The other student had a personal goal and a strong desire to see a specific case that was always scheduled during our didactic lectures, but was finally able to participate in one of these procedures using the hall pass. Both students had expressed how grateful they were to receive the opportunity to participate in their respective cases.
After participation in their “Hall Pass” case, students are asked to write a small written assignment addressing the following as they apply to their case: overview of the case and its uniqueness, what was learned during the experience, what relevant literature is there, and what made this case an important opportunity for you?
We look forward to offering this self-directed learning opportunity for future cohorts of students.
Sustaining Meaningful Education in the Face of COVID-19
As news of COVID19 spread through the nation and medical schools were given the difficult decision on how to offer meaningful education experiences and keep our students on track. For our Phase II medical students, they were removed from campus and clinical learning. UWSMPH and department leaders created a plan to offer an entirely online curriculum through an interim course, which included all didactic learning from all Phase II courses.
Given the circumstances, and a new platform of technology to work with, we have been given a unique opportunity to offer additional meaningful experiences for our Phase II students during this time as well as enhancing our current case discussions with different perspectives.
This is an accordion element with a series of buttons that open and close related content panels.
Didactics
During this interim course we moved all of our SPC case discussions, to Fridays, online, and with 3 cohorts of students in a matter of days – to ride out the time students are prohibited from clinical experiences and to preserve their time for clinic when they are able to return.
With a larger number of learners, we are incredibly grateful to our M4 students, residents, and faculty facilitators who have helped us lead these case discussions online for our students. With their help we have been able breakup the students into smaller groups to go through the case and facilitate more engagement from each student to promote a better learning environment.
Special thanks to the following faculty for being a part of each didactic the past few months –
Dr. Ann O’Rourke & Dr. Lou Bernhardt
Special thanks to the following residents for being reoccurring facilitators for us the past few months –
Taylor Aiken, PGY3R GS
Keon Young Park, PGY3R GS
Special thanks to the following M4 (now PGY1) students for riding out the past few months with us – your future students will be so lucky to have you!
Joseph L’Huillier, MD
Allison Blumenfeld, MD
Albert Perez, MD
Aaron Anderson, MD
New Collaborative Opportunities
As each program within UWSMPH struggled to provide meaningful learning opportunities for students – this perfect storm created a perfect opportunity to seek new interprofessional collaboration opportunities to identify gaps in our current curriculums.
Thanks to our colleagues the PA school – Michelle Ostmoe, Alissa Devos, Amanda Devoss, and members of the MEO – Amy Becker, Gwen Niksic – we were able to come up with a meaningful experience for our MD and PA students in an area that both programs will benefit from this program development.
Medical Student/Physician Assistant Student Quality Improvement – June 15 & 16
This session will provide students with an opportunity to explore how medical errors occur as well as the process for identifying systems issues contributing to the event, in order to prevent future errors.
The goal is for students to understand the purpose of conducting a Root Cause Analysis (RCA) and that participating in a RCA is an important part of being a medical professional.
Most medical errors are systems-based problems and not typically a result of one person’s actions. Therefore, QI is everyone’s responsibility.
Faculty Volunteers/Leaders – Thank you!
Our medical students are beneficiaries of our remarkable department resources. Our residents, fellows, faculty, and administration are composed of dedicated educators that contribute to the success of our students from offering support and mentorship, to sharing their breadth of knowledge and experience.
Thank you to all members of our department for your contributions made to create and sustain an environment that promotes positive educational experiences for our medical students through your day-to-day efforts and for volunteering to help with our Medical Student Curriculum for our M2-M4 students – from assessing student exams, leading didactic learning, orientations, and many other education opportunities during the 2020 academic year – in addition to welcoming a SPC student into your clinic weekly by serving as a continuity clinic preceptor.
Although the pandemic hindered opportunities for our faculty to assist in our Phase 3 curriculum this year – we look forward to involving them in the 2021 academic year – and would still like to recognize and thank the following faculty for their help in the respective Phase 2 learning activities in the Surgical and Procedural Care block.
This is an accordion element with a series of buttons that open and close related content panels.
Orientation Skills Labs - Suture Skills
Dr. Lou Bernhardt has been the focal point of our suturing skills for our Phase II Orientation – and the students are so grateful to being their rotations on SPC with someone who is willing to share all of their wisdom and knowledge to prepare them for the months ahead. Dr. Bernhardt provides the foundational, hands on suturing lessons that our students are able to utilize as members of their teams and improve throughout their time on SPC.
Case Discussions - Facilitators
The following faculty led engaging didactics in relation to their surgical specialties. Each student was given the opportunity to learn foundational content and apply this information through role-playing as physicians in an effort to build cognitive understanding of caring for surgical patients in all specialties – even those they may not have an opportunity to spend clinical time in. In our structured didactics, students are given real (or realistic) case information and asked to work-up the patient from retrieving an H&P, labs, images, and creating differential diagnosis through establishing treatment and adjusting with status updates Our didactics consistently receive high regards given from our students.
| Ken Kudsk | Ann O’Rourke | Daniel Knoch |
| Jim Cole | Robert Redfield | Nathaniel Brooks |
| David Melnick | Brian Gander | Evie Carchman |
| Sarah Jung | Ethan Silverman | Daniel Abbott |
| Tracy Downs | John Hoch | Courtney Morgan |
| Angela Gibson | Greg Hartig | Kristin Long |
| Tabassum Kenedy | Michael Hartung | Jason Stephenson |
| Sarah Johnson | Lee Faucher | Dawn Elfenbein |
| Tiffany Glazer | APPS – Katie Ashburn-Nash, Amy Stacey & Mary Lauby |
Continuity Clinic Faculty Preceptors
As we rounded out our second year of the Forward curriculum transformation and entered our third year, we have seen successful impacts of our Continuity Clinic experiences with our Phase II students, including but not limited to; improved connections, progressive autonomy in clinic, and facilitation of thorough and meaningful feedback.
The Continuity Clinic experience is a recent addition to the clinical experiences offered to our Phase 2 (third year) medical students while they are on the Surgery and Procedural Block. All students are assigned a continuity clinic preceptor based on their expressed interests in a given area/specialty.
The following faculty have welcomed students into their clinic for the duration of the 12-week SPC block in 2019-2020 and contributed to the success of this program. Through their efforts – students are given opportunities to become more familiar with their preceptor’s clinic, which promotes autonomy and progression in the student and an opportunity for faculty to get to know the student better. has been discovered that this longitudinal exposure to students has provided our Phase II students with extensive and meaningful feedback.
Matthew ListerMichael BentzMichael GarrenNathaniel BrooksPamela LangPaul WhitingRay KingRobert RedfieldSamuel PooreShilpa ReddySusan PittTom PasicTracy DownsVic WeissSean Ronnekleiv-Kelly
| Aaron Wieland | Andrea Spiker | Angela Gibson |
| Anne Lidor | Brett Michelotti | Brian Gander |
| Catharine Garland | Christopher Doro | Courtney Morgan |
| Cristina Geltzeiler | Dan Abbott | Daniel Knoch |
| David Francis | David Melnick | David Upton |
| Dawn Elfenbein | Elise Lawson | Gregory Hartig |
| Heather Potter | Jake Greenberg | James Stadler |
| Jennifer Larson | Jessica Van Beek-King | John Scarborough |
| Josh Mezrich | Katherine Gast | Kristin Long |
| Kyle Richards | Lee Faucher | Mahua Dey |
OSCE Assessors
The OSCE is a multi-station objective structured clinical examination. This is given at the end of the SPC block and assessors grade students in-person or remotely on their clinical skills.
| Lou Bernhardt | Amber Shada | Ashley Anderson |
| Hee Soo Jung | David Melnick | Ken Kudsk |
| Ian Koszewski | Dawn Elfenbein | Jerry Lang |
| Gregory Hartig | David Al-Adra | Ann O’Rourke |
| John Scarborough | Angie Ingraham | Paul Staskowski |
| Courtney Morgan |
Unanticipated Outcomes DTA - SPC Integration *NEW THIS ACADEMIC YEAR*
During this session, our Phase 2 medical students will participate in 2 standardized patient encounters in which they will deliver news regarding an error to a patient or family member via telehealth.
Each student will participate as the Acting MD in one of the two cases, and swap and observe their peers participation in the other case.
Our volunteers served as facilitators for this exercise and promoted student learning through experience and reflection.
| Nathaniel Brooks | Mahua Dey | Becky Sippel |
| Ann O’Rourke | Irina Shakhnovichk | Amber Shada |
| Tracy Downs | Thomas Pasic | Lou Bernhardt |
Phase II Interm Course Online CBL Didactic / March - June 2020 (COVID-19) *NEW THIS ACADEMIC YEAR*
Due to the COVID19 pandemic, our medical students were kept from clinical learning experiences for three months and spent this time completing all of the didactics for each block in Phase II entirely online. Given the circumstances, we have been given a unique opportunity to build on our didactics and to offer additional meaningful experiences for our Phase II students during this time. The following residents have helped us facilitate and design our lessons during this time:
| Mahua Dey | Ann O’Rourke | Irina Shakhnovich |
| Lou Bernhardt | Mason Fisher | Daniel Knoch |
| Karin Zuegge | Alian Aquino | Adrian Pichurko |
| Jennifer Larson | Dawn Elfenbein | David Melnick |
| Jim Cole | Evie Carchman | Lee Faucher |
| Tiffany Glazer | John Hoch | Tracy Downs |
Phase III (Medical Specialties & Residency Prep)
Phase III | Career Exploration and Preparation
16 Months | January – May
This is an accordion element with a series of buttons that open and close related content panels.
Phase 3 Surgery Leadership

IAI – Course Director

IAI – Course Director

IPC – Course Director

IAI – Course Director
IPC – Course Co-Director
Thank you to the following faculty for serving as educational leaders within your divisions and for your contributions to our medical student education in both Phase II and III:
General Surgery
Blue Team- Sean Ronnekleiv-Kelly
Gold Team – Amber Shada
Green Team – Lee Faucher
Orange Team – Chip Foley
Pediatric Team – Adam Brinkan
Red Team – David Melnick
VAH Team – Christina Geltzeiler
Cardiac – Amy Fiedler
Thoracic – Daniel McCarthy
Otolaryngology – Greg Hartig
Plastics – Venkat Rao – *now Del Mount
Transplant – Robert Redfield
Vascular – Paul DiMusto
Anesthesia – Karin Zuegge
Interventional Radiology – Mark Kleedehn
Neurosurgery – Nathaniel Brooks
Ophthalmology – Dan Knoch
Urology – Tracy Downs
Surgery Electives and Inpatient Acting Internships
The ForWard Curriculum gives students in Phase III an opportunity for advance clinical experiences, career exploration and to build relationships with faculty. There are currently two options for students in this phase to rotate on our surgical services that offer different experiences. Each course offers advanced learning opportunities for better internship preparation.
Electives
Phase III students have the option to explore our services in two or four-week elective courses. These courses are organized in such a way that gives students an opportunity to gain advanced clinical experience, explore different career options and receive letters of recommendation from our renowned faculty as they prepare for the upcoming residency match. Students on a service for four weeks will complete an audition rotation through this elective.
Inpatient Acting Internships
Much like elective courses, Phase III students have the option to explore our services in a four-week rotation by gaining advanced clinical experiences. An Inpatient Acting Internship is a graduation requirement for UWSMPH. Faculty across UWSMPH collaborate on a core skill-building orientation for students enrolled in this course. Students have the opportunity to receive letters of recommendation from faculty and complete an audition rotation through their Inpatient Acting Internship. The students in this course have additional requirements to increase their clinical and interprofessional skills.
Internship Preparation Course
Graduating Phase III students participate in a two-week Internship Preparation Course (IPC) where they review key concepts and practice essential skills to ensure success as they transition out of medical school. The curriculum includes knowledge-based, skills-based, and pragmatic guidance regarding topics such as writing orders, patient handoffs, communication, and professionalism. Faculty across UWSMPH collaborate on this course and provide an excellent opportunity for medical students before they become interns.
Basic Science Selectives
- Aortic Disease from Bench to Bedside – Course Directors: Courtney Morgan, MD & Bo Liu, PhD
- Aortic Disease from Bench to Boardroom – Course Directors: Courtney Morgan, MD & Bo Liu, PhD
- The Science of Obesity & Diabetes – Course Directors: Amber Shada, MD & Michelle Kimple, PhD
- Somethings Wrong With My Butt! Common Colorectal Diseases – Course Director: Ray King, MD, PhD
Public Health Selectives
- Optimizing Value, Quality, and Safety in Health Care – Course Directors: M. Gretchen Schwarze, MD, John Scarborough, MD, & Jonathan Kohler, MD
- Patient Education as a Strategy for Advocacy – Course Directors: Sarah Jung, PhD & Hee Soo Jung, MD
- Multidisciplinary Approaches to Colon Cancer Prevention & Treatment – Course Director: Evie Carchman, MD
- Injury & Violence Prevention – Course Director: Ann O’Rourke, MD
Faculty Volunteers / Leaders – Thank you!
Thank you to all the faculty, residents, and staff who help our Phase III students as they explore surgical specialties for their career. They truly appreciate it!
Successes
Our Department’s surgery clerkship has made great strides in improving our medical students’ educational experience, as demonstrated in the 2019 AAMC Medical School Graduate Questionnaire results. Our scores rose notably, especially in the areas of observing history (73.6% in 2018 to 90.3% in 2019), physical examinations (83.6% in 2018 to 91.6% in 2019), and mid-clerkship feedback (93.7% in 2018 to 98.7% in 2019). Congratulations to the Director of Medical Student Education, Ann O’Rourke, MD, MPH, and her team, and Dorothy Cook, MS, for their hard work. Thank you to all the faculty, residents, and staff for their continued dedication to medical student education! Access the report here.
Match Data
Number of UWSMPH Students Matching into Surgical Specialties: 2000 – 2020
| 00 | 01 | 02 | 03 | 04 | 05 | 06 | 07 | 08 | 09 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General Surgery |
9 | 4 | 9 | 7 | 10 | 7 | 4 | 7 | 7 | 13 | 14 | 7 | 9 | 14 | 10 | 11 | 8 | 11 | 8 | 4 | 8 |
| Surgery – Prelim |
8 | 2 | 6 | 4 | 0 | 12 | 7 | 1 | 7 | 4 | 6 | 6 | 8 | 5 | 4 | 1 | 3 | 0 | 0 | 0 | 2 |
| Orthopedic | 2 | 3 | 1 | 2 | 3 | 3 | 4 | 10 | 6 | 5 | 5 | 5 | 6 | 6 | 6 | 12 | 5 | 8 | 3 | 5 | 5 |
| Otolaryn -gology |
1 | 3 | 2 | 0 | 0 | 3 | 3 | 2 | 3 | 3 | 0 | 0 | 3 | 2 | 2 | 7 | 3 | 2 | 1 | 0 | 4 |
| Plastic Surgery |
0 | 3 | 0 | 0 | 2 | 1 | 0 | 0 | 1 | 2 | 1 | 0 | 1 | 2 | 3 | 1 | 3 | 1 | 1 | 3 | 2 |
| Vascular | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 0 |
| Urology | 4 | 1 | 2 | 1 | 1 | 0 | 2 | 0 | 1 | 0 | 1 | 2 | 1 | 3 | 3 | 0 | 0 | 2 | 3 | 1 | 2 |
| 24 | 16 | 20 | 14 | 16 | 26 | 20 | 20 | 25 | 27 | 27 | 20 | 28 | 32 | 28 | 32 | 23 | 24 | 17 | 14 | 23 |