By Dr. Tony Kille
Three years ago, the otolaryngology service noticed some problems with the immediate postoperative cares of pediatric patients undergoing tracheostomy. This came to light after several patients were noted to have problematic skin breakdown at the tracheostomy site. In addition, our team was getting frequent, frustrated calls from the pediatric ICU — “the trach straps are too tight,” “the dressing is not looking right,” “when will we be doing the first trach change?” I was discussing these issues with Dr. Dylan Lippert as we were doing a case one day at the American Family Children’s Hospital — he was a junior resident at that time, and he was often on the receiving end of those frustrated PICU calls. After comparing notes, we decided to tackle the problem in a more comprehensive fashion. Thus, our pediatric postoperative tracheostomy care quality improvement project was born.
We started this QI project by examining our current tracheotomy technique and postoperative care protocols. We identified variations in our practices that could be related to the skin breakdown issue. Specifically, there were inconsistencies in how tracheostomy tubes were secured, daily wound cares, and the timing of the first tracheostomy tube change. We also examined the medical literature to identify “best practices” and possible solutions. Our goal was to incorporate practices that would decrease skin breakdown while not compromising patient safety. This led to the creation of a new standardized protocol for immediate postoperative care of pediatric tracheostomy patients, which was initiated in February 2012.
The elements of the standardized pediatric tracheostomy care protocol include:
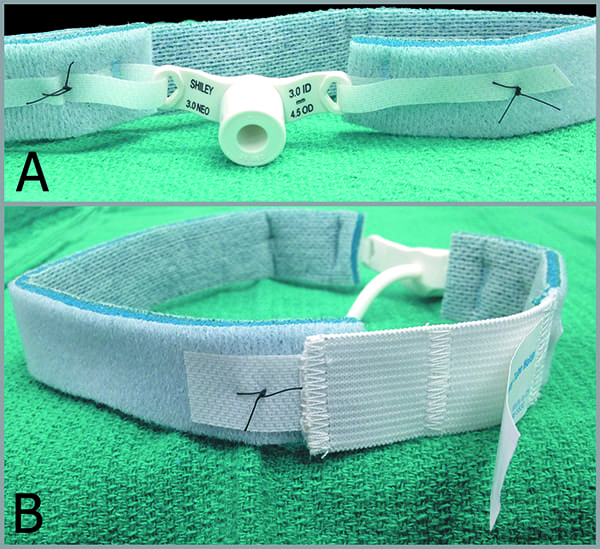
- Securing tracheostomy tubes with soft foam straps rather than twill ties. A suture is placed through the strap at all adjustable sections so tension could not be altered. (Figure 1).
- Placing a split drain sponge under the tracheostomy tube in the OR and daily changing by the rounding otolaryngology team.
- Performing the first tracheostomy tube change at the bedside in the PICU on postoperative day three or four.
- Not changing surgical technique. Most patients underwent a standard pediatric tracheotomy (vertical skin incision, horizontal tracheal incision, formal stoma creation), but patients older than 12 years of age underwent an “adult style” tracheotomy with an inferiorly based Bjork flap.
The outcome
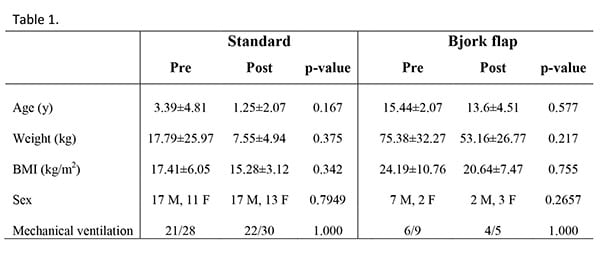
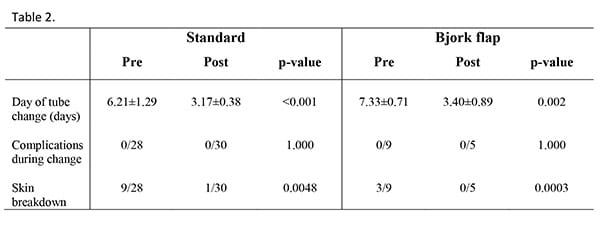
After instituting the standardized care protocol, we have monitored outcomes, focusing on rates of skin breakdown as well as overall complications. We’ve compared outcomes in patients undergoing tracheostomy two years before introducing the standardized protocol with those undergoing tracheostomy two years after. Patient characteristics are detailed in Table 1. Thirty-seven patients in the pre-protocol group and 35 in the post-protocol group were analyzed. The rate of skin breakdown was significantly lower in the post-protocol group (standard: p=0.0048; Bjork flap: p=0.0003). Later tracheostomy tube change was associated with an increased rate of skin ulceration (standard: OR=2.040, p=0.003). In the post-protocol group, all tube changes were safely accomplished on postoperative day three or four, and the stomas were deemed to be adequately matured to do so in all cases. No major complications were noted in either the pre-protocol or post-protocol groups. Comparison of complication rates are detailed in Table 2.
A significant number of children did develop areas of skin breakdown related to the placement of their tracheostomy tube prior to institution of our standardized postoperative care protocol. Skin breakdown related to tracheostomy is especially common in pediatric patients because their skin is more delicate, and the percent of body surface area covered by the tube and securing straps is greater than in adults. Children are often unable to effectively communicate discomfort related to pressure. Skin-related complications occur most often during the immediate postoperative period, when the tracheostomy tube is secured most tightly1.
Prevention of skin breakdown of course has several benefits:
- An open wound is a potential source of infection and leads to increased use of health care dollars, including the need for wound care specialists and increased length of hospital stay.
- Open draining wounds increase caretaker resistance to learning tracheostomy care, also extending inpatient stays
- Children with skin ulceration at the tracheostomy site likely experience more pain with routine tracheostomy cares and tube changes.
Performing the first tracheostomy tube change as early as possible is desirable, but the stoma must be mature to safely change the tube without risking creation of a false passage. A stoma is mature when the tract has epithelialized, and the open edges of the tracheal wall have secured to the subcutaneous tissues 2. Formally maturing the stoma at the time of surgery, as was done for all of our patients, has been shown to decrease accidental decannulation and traumatic recannulation in pediatric patients 3. Little has been published regarding timing of the first tube change in relation to complications; rather, this is often based on tradition and the surgeon’s availability. A recently published consensus advocates waiting 5 to 7 days in pediatric patients in order for the stoma to mature 4. One report, published by Deutsch in 1998, noted adequate stomal maturation and no complications when performing the first tracheostomy tube change in pediatric patients at the bedside on postoperative days three or four 5.
Our data support Deutsch’s assertion that a pediatric tracheostomy stoma is adequately mature by postoperative day three, and that it is safe to perform the first tube change at that time. Benefits of earlier tube change include:
- Earlier mobility of the patient, reducing potential for decubitus ulcer formation
- Shorter periods of sedation/ventilation and thus a lower risk of ventilator-associated pneumonia
- Earlier transfer from intensive care to general care
- Earlier initiation of rehabilitation activities such as physical therapy
- Earlier caregiver education and hands-on practice
We are pleased with the results of our quality improvement project thus far, and we continue to follow the standardized care protocol. However, we will continue to monitor outcomes and look for ways to keep improving.
Citations
1 K. Bressler, L. Coladipietro, L.D. Holinger. Protection of the cervical skin in the pediatric patient with a recent tracheostomy, Otolaryngol. Head Neck Surg. 116(3) (1997) 414-415.
2 R.M. Perkin. Pediatric Hospital Medicine: Textbook of Inpatient Management. 2nd ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008.
3 J.Y. Park, D.L. Suskind, D. Prater, H.R. Muntz, R.P. Lusk. Maturation of the pediatric tracheostomy stoma: effect on complications, Ann. Otol. Rhinol. Laryngol. 108(12) (1999) 1115-9.
4 R.B. Mitchell, H.M. Hussey, G. Setzen, et al. Clinical consensus statement: tracheostomy care, Otolaryngol. Head Neck Surg. 148(1) (2013) 6-20.
5 E.S. Deutsch. Early tracheostomy tube change in children, Arch. Otolaryngol. Head Neck Surg. 124(11) (1998) 1237-1238.