This article first appeared in the ‘Quarterly,’ The Magazine for alumni, friends, faculty, and students of the University of Wisconsin School of Medicine and Public Health. See the complete issue, along with the original layout of this article, HERE.
The year was 1924. The first Winter Olympics were held in the French Alps town of Chamonix, and the inaugural Macy’s Thanksgiving Day Parade passed through Herald Square in Manhattan. Calvin Coolidge, who had assumed the presidency following the death of Warren Harding, was victorious in the presidential election. The first successful around-the-world flight, spanning 175 days and 27,553 miles, was completed. And University of Wisconsin–Madison established the Department of Surgery at the UW Medical School [now the UW School of Medicine and Public Health (SMPH)].
When the campus leaders converted the UW Medical School from a two-year to a four-year school in 1924, Charles Bardeen, MD, dean of the medical school, created only two clinical departments: the Department of Surgery and the Department of Medicine. The Department of Surgery consisted of three full-time faculty members: Carl Hedblom, MD, the inaugural chair of the department with an annual salary of $8,000, and Albert Crawford, MD, and B.H. Hager, MD, both associate professors with annual salaries of $5,000 each.
Since those humble beginnings, the Department of Surgery has grown to more than 170 full-time faculty members and nearly 200 staff members across 11 divisions. The department was established in conjunction with the opening of Wisconsin General Hospital at 1300 University Avenue. Fifty-five years later, UW Hospital opened at its current location on the west end of campus. Today, Department of Surgery faculty members practice at five clinical sites in Madison, as well as several clinical outreach sites throughout Wisconsin and northern Illinois.
The department is highly ranked among its peers in the United States, explains Michael Bentz, MD, the Layton F. Rikkers, MD, Chair of Surgical Leadership and a professor in the Departments of Surgery, Pediatrics, and Neurosurgery, who has been a member of the faculty since 1999. He says, “Every surgery department has a mission of clinical care, research, and education. We do all those things well and have continued to improve them over the years.”
Innovation at the Forefront
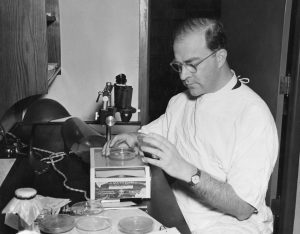
Many of the Department of Surgery’s research breakthroughs are well-documented and have helped shape the medical world. In 1938, Frederic Mohs, MD ’34, pioneered a skin-cancer treatment technique that is still in widespread use today. By dissecting tumors and examining them microscopically during surgery, the procedure — called Mohs Surgery — leaves as much healthy tissue in place as possible and reduces scarring after the removal of cancerous cells. Prior to Mohs Surgery, skin cancer was treated by making a wide surgical excision, which often resulted in significant deformity.
In the 1970s and 1980s, a research team led by Folkert “Fred” Belzer, MD, and James “Jim” Southard, PhD, began exploring organ preservation, leading to a development that changed the field of transplantation forever: the UW Solution, which significantly extends the viability of donor organs. Prior to the UW Solution, a liver from a brain-dead donor had to be implanted within four to six hours of retrieval. With the use of the UW Solution, preservation time is extended to 20 hours. This was revolutionary, as location no longer had an influence on who could receive an organ. Today, nearly 40 years since the UW Solution was created, transplant centers around the world still use it to preserve kidneys, livers, pancreases, and intestines. This discovery has saved thousands of lives.
“Our department has a very strong tradition of having a significant impact in various disciplines of surgery,” notes Luke Funk, MD, MPH, FACS, an associate professor in the Department of Surgery’s Division of Minimally Invasive Surgery and the department’s vice chair of research. “You name the division, and I think we’ve had important contributions in each of the areas.”
That spirit of innovation lives on today with a research portfolio topping $18 million, nearly 50 active labs, and state-of-the-art programs and facilities, including the Wisconsin Surgical Outcomes Research Program. Collaboration across the SMPH and UW–Madison — such as the creation of the Center for Biomedical Swine Research — is the hallmark of current research projects and will continue to lay the groundwork for breakthroughs.
“One of the remarkable things about the culture here is how much we subscribe to the Wisconsin Idea,” observes Muhammed Murtaza, MBBS, PhD, an associate professor in the Division of Surgical Oncology and the director of the Center for Human Genomics and Precision Medicine. “For me, the essence of the Wisconsin Idea is that what we do isn’t about academic productivity for its own sake, but really about how what we’re doing [will have] an impact on the real world.”
Clinical Care Central to the Mission

By all accounts, the Department of Surgery rose to national prominence as a top clinical department under the leadership of Belzer, who served as the department chair from 1974 to 1995. In conjunction with work on the UW Solution, he is credited with developing a world-class Division of Transplantation Surgery within the department.
Belzer was succeeded as chair by Layton “Bing” Rikkers, MD, FACS, who oversaw tremendous growth of the department, including the rise of sub-specialties. Under Rikkers, the faculty more than doubled in number; his recruitment centered around skilled surgeons.
“Above all, Dr. Belzer believed in excellence in clinical surgery. He made sure that his faculty were superb surgeons, and he recruited that way,” recalls Bruce Harms, MD, MBA, FACS (PG ’83), emeritus professor and former head of the Division of Colorectal Surgery. “And that trend continued when Dr. Rikkers arrived. He put the University of Wisconsin on the radar screen nationally in a way we had never seen before.”
Belzer and Rikkers ushered in many advances in clinical care. For instance, the dream of organ transplantation became a reality at UW–Madison in 1966, when faculty members performed the first kidney transplant. Seven years later, a headline in Madison’s Capital Times newspaper read, “Heart Transplant is Performed at U. Hospital.” And in 1984, the Liver Transplant Program began, followed in 1988 by the first lung transplant. Today, UW Health’s Transplant Program is one of the most experienced in the United States, with the Pancreas Transplant Program among the most highly ranked nationwide. In April 2024, the UW Health Transplant Center reached a milestone of 20,000 organs transplanted.
In the late 1990s, Rikkers recruited Dennis Lund, MD, to build a pediatric surgery program. Lund was a driving force behind the creation of American Family Children’s Hospital, which opened in 2007. Petros Anagnostopoulos, MD, MBA, FACS — a professor in the Division of Cardiothoracic Surgery and the surgeon in chief at American Family Children’s Hospital — later helped launch the nationally recognized Pediatric Cardiology and Heart Surgery Program. In August 2023, surgeons performed UW Health’s first pediatric heart transplant.
“I think the most important thing for clinical care is that we never have lost sight of the fact that there’s a patient at the center,” says Rebecca Minter, MD, MBA, FACS, the A.R. Curreri Distinguished Chair and Professor, Department of Surgery. “We need to care about patients and not just care for them. That moment in time for them is something that is perhaps the most difficult time in their life, and they will remember this interaction forever. We need to make sure we create an environment where that patient experience is always held front and center.”
Education at the Core

Education has always been central to the Department of Surgery’s mission. Since the first general surgery resident graduated in 1925, thousands of residents and fellows have trained in Madison. Today, the department’s nationally recognized and competitive graduate medical education programs consist of four residencies (general surgery, otolaryngology, plastic surgery, and vascular surgery) and 10 fellowship training programs, accounting for nearly 120 trainees per year.
“Being an educator and getting somebody through that cycle is incredibly rewarding,” states Ann O’Rourke, MD ’02, MPH ’06, FACS (PG ’09), an associate professor in the Division of Acute Care and Regional General Surgery and the program director of the General Surgery Residency Program. “We are training leaders in [domestic] and global surgery. The Wisconsin brand means something. Our residents, when they go out and do fellowships or get jobs, are very well-regarded, and that says a lot about the training they get here.”
More than 45 current faculty members, spanning all 11 divisions, completed at least part of their post-graduate training with the Department of Surgery and returned to the full-time faculty. They credit the culture of the department and the respect that is shared among trainees and teachers.
“Since the first day I was an intern, I felt nothing but a sense of family, a sense of warmth, a passion for excellence,” reflects Adam Brinkman, MD (PG ’15), an associate professor in the Division of Pediatric Surgery and the pediatric trauma medical director for American Family Children’s Hospital. “I really was sad on my very last day [of my residency]. As I walked out of the hospital, I said to myself, ‘One day I’m going to come back and be a part of this family.’ I had that opportunity and returned in 2017, and it’s where I’m going to finish my career. There’s no other place that I would rather work than the University of Wisconsin.”
Looking Ahead
A hundred years after its founding, the Department of Surgery within the SMPH is one of the leading academic surgical programs in the nation. Department faculty members perform almost 22,000 operations each year and advance a robust research portfolio. Over the past decade, compared to other surgery departments, the SMPH Department of Surgery has been highly ranked for National Institutes of Health funding, totaling nearly $130 million from 2014 to 2023.
“I am excited for the future,” says Minter. “We are delivering cutting-edge surgical care across 11 divisions and are pursuing innovative educational strategies. Not only do we have incredible talent in this department, but we have built a vibrant, collaborative culture that is a wonderful training ground for the next generation of health care leaders.”