Written by colorectal surgeon Cristina Geltzeiler, MD
What is a malignant polyp?
A malignant polyp is a colon or rectal growth that has been entirely or partially removed with colonoscopy that contains cancer cells.
What to do first?
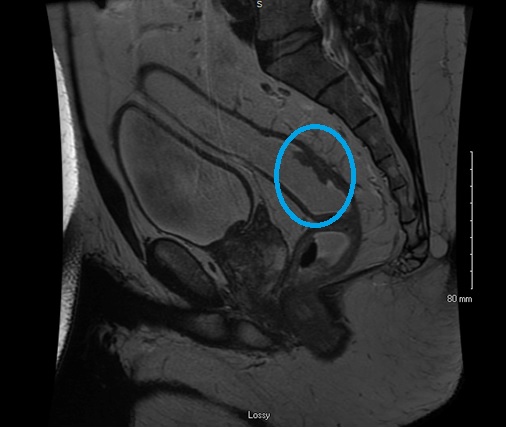
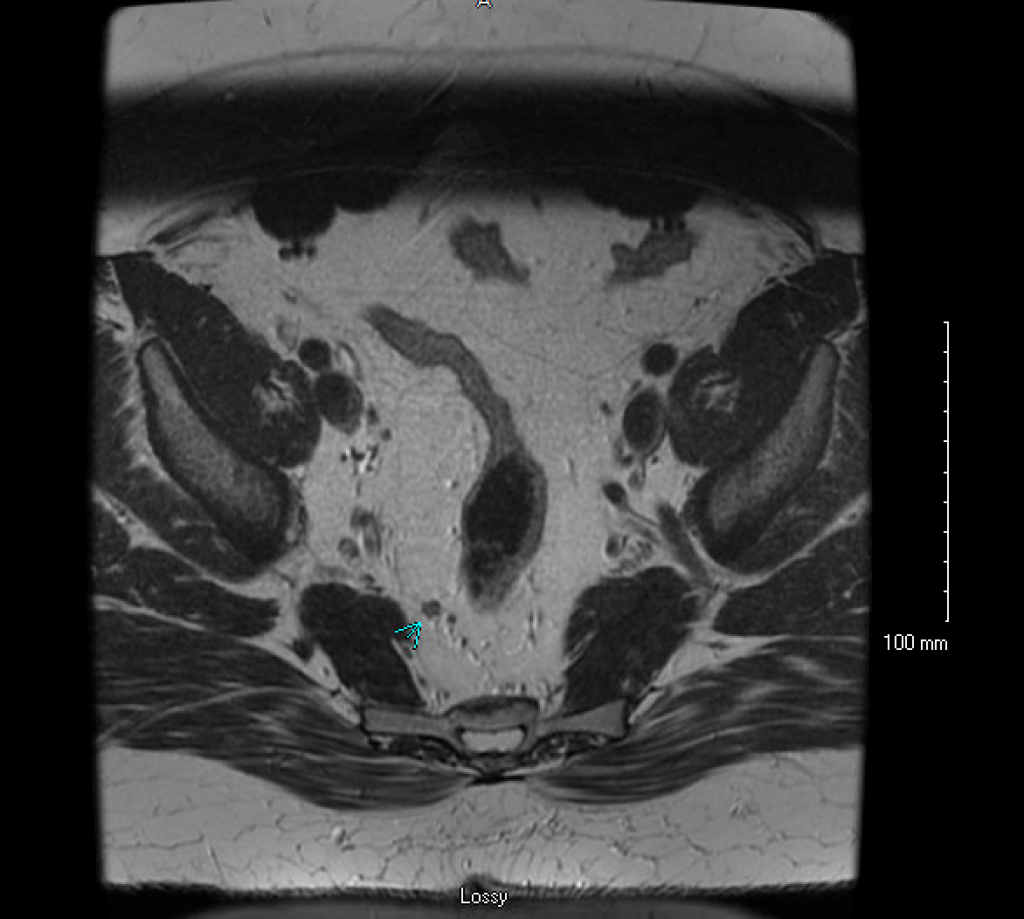
First and foremost, it is important to remember that this is a cancer and it should be staged appropriately. The most common malignant polyps contain cancer cell type called adenocarcinoma. The work-up for these includes computed tomography (CT) scan of the chest, abdomen and pelvis along with carcinoembryonic antigen (CEA) level. Importantly, if the area has not been marked colonoscopically with an intraluminal tattoo this should be done. Preferably this is done within the first 2 weeks when the scar is still visible. If the malignant polyp is within the rectum, local staging is also indicated. This is performed utilizing an endorectal ultrasound (EUS) or rectal protocol magnetic resonance imaging (MRI), Figure 1. It is important to note that these pelvic imaging tests are specialized. Many medical centers do not have the capability to perform specialized rectal protocol MRI or the expertise to perform endorectal ultrasound. If there is any question as to testing to be ordered for rectal cancer, consultation with a colorectal surgeon is encouraged.
Staging work-up complete – now what?
In the absence of metastatic disease, the main question becomes – is the polypectomy enough or does the patient need further treatment? Options at this point become:
- Observation with ongoing surveillance
- Repeat local excision
- Formal oncologic resection (colectomy or proctectomy with lymphadenectomy)
In order to answer the question of which approach is most appropriate, we need to understand the risk of lymph node metastases. If the patient has a high risk of lymph node metastases, a formal oncologic resection is typically recommended.
Risk of Lymph Node Metastases
The overall risk of lymph node metastases for a T1 colorectal cancer (into the submucosal layer of the bowel but not into the muscularis propria) ranges from 6-13%. The key component to determine if the patient needs a formal resection is to establish if they are at high or low risk of lymph node metastases.
Two classification schemes that are utilized are the Haggitt classification (for pedunculated (on a stalk) polyps) and the Kikuchi/Sm classification (for sessile (flat) polyps). These classification schemes determine the depth of the cancerous component of the polyp into the submucosa which therefore correlate with risk of lymph node metastases. Haggitt levels 1-3 and Kikuchi/Sm level 1 correlate with a low risk of lymph node metastases (~1-3%), whereas Haggitt level 4 and Kikuchi/Sm levels 2-3 correlate with a high risk of lymph node metastases (8-27%). In general, most would recommend formal resection in those with high risk of lymph node metastases in acceptable operative risk candidates.
Other factors to consider when determining risk of lymph node metastases:
1. Close or positive margins
– Many would consider this inadequate local treatment
– < 1mm margin is considered “positive”
2. Lymphovascular invasion
3. Poorly differentiated histology (Grade 3)
4. High level of tumor budding
– 0-4 Low
– 5-9 Intermediate
– 10+ High
5. Rectal location (3rds) versus colon location
– As a general rule, the more distal the cancer the more likely that lymph nodes will be positive
It is important to note that in order to get these pathologic details that are critical in decision making, the clinician may need to request a more detailed pathology report, often referred to as a synoptic report.
Features to suggest local excision is enough
- Haggitt levels 1-3 or Sm level 1
- Well-differentiated histology
- No lymphovascular invasion
- Single resection (non-piecemeal) with a negative margin
Although lymph node involvement is rare in these highly selected patients it is important to remember it is NOT zero and surveillance for lymph node metastases is challenging (rectal) to extremely difficult (colon).
Features to consider formal resection is indicated
- Haggitt level 4/Sm level 3
- Poorly-differentiated histology
- Lymphovascular invasion
- Piecemeal resection or positive margin
Colon and rectum treated differently
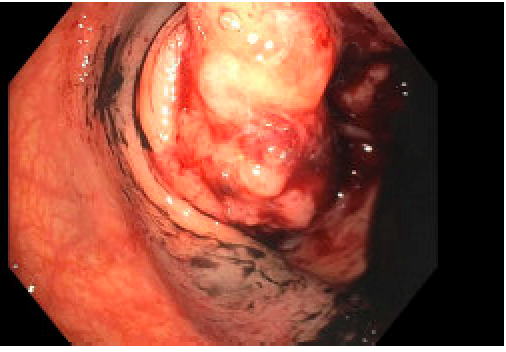
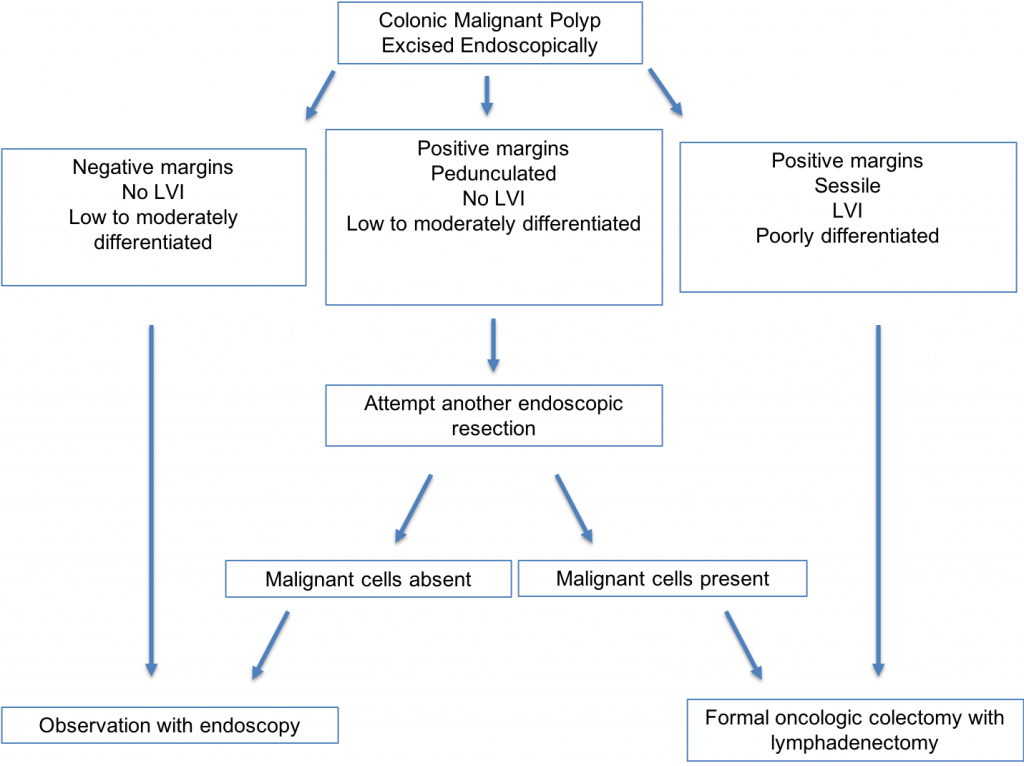
The algorithm for treating malignant colon polyps is fairly straightforward, as depicted in Figure 2.
Malignant rectal polyps are much more complex. Factors at play include the:
- High risk for nodal metastases compared to colonic malignant polyps, but better ability to predict with local staging (MRI or EUS)
- High operative morbidity and effect to patient quality of life associated with oncologic rectal resection, which may include temporary or permanent ostomy
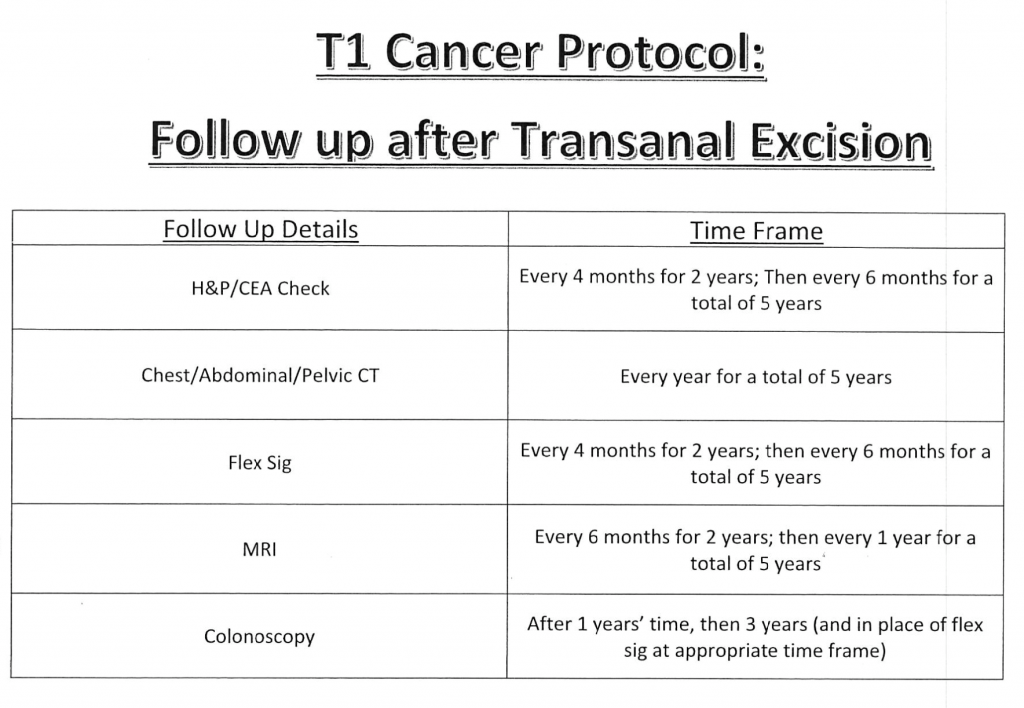
- Rigorous surveillance is needed if opt for non-oncologic excision, Figure 3.
- More operative options including open local excision and minimally invasive local excision techniques: Transanal endoscopic Microsurgery (TEM) and Transanal Minimally invasive surgery (TAMIS)
- If there is any question regarding the management a malignant rectal polyp, it should be discussed in a multidisciplinary setting. It is our practice at the University of Wisconsin to discuss all of these in this manner.
A note about endoscopic practices
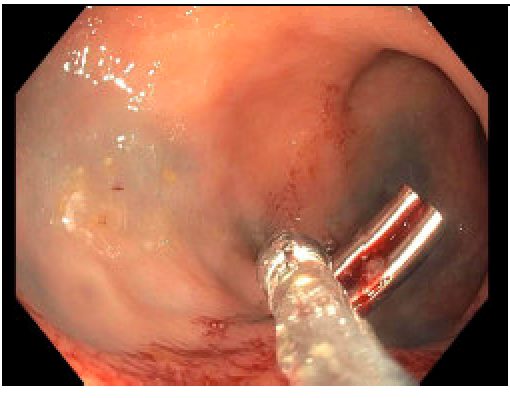
1. Clips: Clips should be utilized sparingly in the rectum. It is rarely necessary to close the mucosal defect from a polypectomy in the rectum. The majority of the rectum is extraperitoneal, making even full thickness rectal defects of little clinical consequence. Even “MRI compatible” clips preclude rectal MRI staging due to the significant scatter artifact they cause for MRI imaging. These clips often stay for a prolonged period of time and sometimes need to be endoscopically removed in order for MRI to be scheduled, Figure 4. This can delay patient work-up for their cancer.

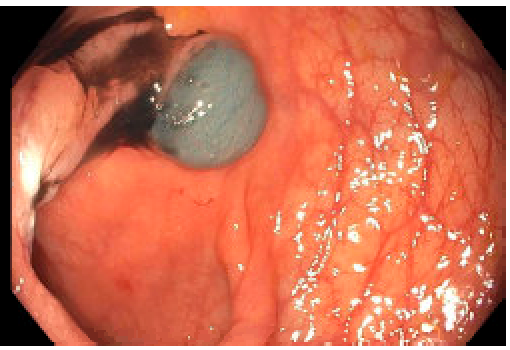
2. Tattoos: Techniques for tattooing in the colon should be different than those in the rectum, Figure 5.
- In the colon, if endoscopic tattooing is indicated for planned colectomy, it is preferable to tattoo in at least 2 quadrants. It is impossible to tell with colonoscopy which quadrant the mesentery is in. If only the mesenteric quadrant is tattooed this may not be visible to the operative surgeon.
- In the rectum, a more pointed spot tattoo is typically preferred. If a local excision is planned, a pointed tattoo will assist the surgeon in finding the often very small scar, which can be difficult to find with diffuse tattooing. Additionally, if neoadjuvant chemoradiotherapy indicated after local staging performed, a pointed tattoo will help the surgeon identify the distance of the lesion in the setting of a complete clinical response.
Additional Considerations
– Take into account patient’s overall health status – can they tolerate a major abdominal operation?
– Educated discussion with patients about risk of nodal metastases and patient preferences taken into account – especially with early low risk rectal cancers
– Adhere to strict follow-up surveillance when forego formal resection
Conclusion
In conclusion the management of a malignant colorectal polyp depends on multiple factors. The care of these patients depends on the expertise of endoscopists, pathologists, radiologists and surgeons.
Learn more about colorectal surgery services at UW Health
Our colorectal surgery program is the largest in Wisconsin. Learn more about our providers and the range of services we provide, and how to refer patients.
Want more updates like this?
Sign up to receive clinical updates from the UW Department of Surgery by joining our email list.
References
1. Butte JM, Tang P, Gonen M, et al. Rate of residual disease after complete endoscopic resection of malignant colonic polyp. Dis Colon Rectum. 2012;55(2):122-127.
2. Hassan C, Zullo A, Risio M, Rossini FP, Morini S. Histologic risk factors and clinical outcome in colorectal malignant polyp: a pooled-data analysis. Dis Colon Rectum. 2005;48(8):1588-1596.
3. Nascimbeni R, Burgart LJ, Nivatvongs S, Larson DR. Risk of lymph node metastasis in T1 carcinoma of the colon and rectum. Dis Colon Rectum. 2002;45(2):200-206.
4. Nivatvongs S, Rojanasakul A, Reiman HM, et al. The risk of lymph node metastasis in colorectal polyps with invasive adenocarcinoma. Dis Colon Rectum. 1991;34(4):323-328.
5. Seitz U, Bohnacker S, Seewald S, et al. Is endoscopic polypectomy an adequate therapy for malignant colorectal adenomas? Presentation of 114 patients and review of the literature. Dis Colon Rectum. 2004;47(11):1789-1796; discussion 1796-1787.