
Musicians, athletes, and even business executives use coaching to improve performance. Why not surgeons? While we may not associate coaching with surgery, Caprice Greenberg, MD, MPH, and her team in the Wisconsin Surgical Outcomes Research (WiSOR) program, including Jacob Greenberg, MD, Jessica Schumacher, PhD, MS, and Sudha Pavuluri Quamme, MD, MS, are pursuing innovative research to explore how to make coaching available to more surgeons.
This research recently received a five-year, $1.9 million R01 grant from the Agency for Healthcare Research and Quality (AHRQ) and is a collaboration with the Americas Hernia Society Quality Collaborative (AHSQC) led by Dr. Benjamin Poulose and Michael Rosen.
The investigation, entitled “Video-based Collaborative Learning to Improve Ventral Hernia Repair,” will compare two approaches that use video-based feedback to help surgeons improve their surgical performance in ventral hernia operations. The goal of the project is to develop new approaches for collaborative learning that can improve surgical quality and close the performance gap between surgeons.
Surgical Performance Matters
Research has shown that individual surgeon performance affects patient outcomes considerably due to variations in the steps a surgeon uses to complete the operation as well as in the surgeon’s technical skills. Surgical coaching can be an effective way of improving surgeon performance, but this promising intervention faces a significant barrier.
“Despite the fact that surgeons recognize the importance of surgical quality improvement, time presents a real problem for them,” said Dr. Greenberg. “Face-to-face interactions between surgeons and coaches—who are both very busy clinically—are time-intensive and difficult to coordinate. This has made it challenging to implement surgical coaching in a widespread way.”
The two interventions proposed in this study are designed to overcome this challenge and provide an effective, time-efficient approach to giving feedback on their operations. Previously, the project’s research team has had success offering surgeons face-to-face coaching sessions during professional meetings they already attend. The team also believes the internet can offer an opportunity for collaborative learning while limiting the need for time-intensive face-to-face meetings.
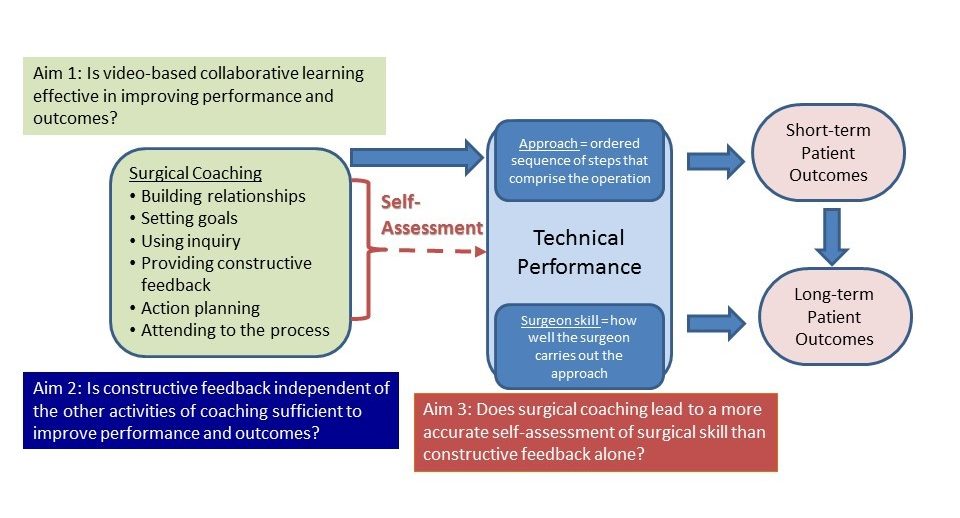
Based on these ideas, the research team will test the effectiveness of two interventions that provide surgeons with constructive feedback: live in-person coaching and post-surgery feedback using a web-based platform. The goal of both interventions is to use video review to help surgeons adopt new approaches, improve their technical and communication skills, and ultimately, have a significant impact on patient outcomes.
Focusing on Hernias
Abdominal wall hernias are among the most common surgical disorders, with over 350,000 US patients requiring repair annually. Despite this prevalence, outcomes remain poor and vary widely. Hernias recur at rates that range between 32% and 63% at 10 years. Interestingly, recurrence rates between surgeons differ significantly, with rates for some surgeons 5 times higher than those of their peers.
Part of the problem is that new repair techniques and advances in biomedical devices and technology are constantly evolving. It’s difficult for surgeons to stay up to date on new developments and incorporate advances into their practice. Because hernia repairs are such common operations, and vary in their success, they’re the ideal operations with which to study the impact of surgical performance as well as to develop interventions that can improve it.
Pairing Surgeons with Coaches
Fifty-four surgeons from across the United States will participate in the study. Each surgeon will be paired with a coach to collaboratively review their hernia repairs. All participants in the program will submit two videos of their surgeries: the first before the intervention, and the second after they receive feedback (either through face-to-face coaching or internet-based video review). These videos will then be assessed by other surgeons using a method to measure their technical skill and provide an intermediate outcome to patient complications and hernia recurrence.
The first group will participate in a live video-based coaching session and meet face-to-face with their coach at three national meetings. The second group will take part in a web-based program in which a coach reviews video footage of the surgery and offers comments without any real-time interaction. The surgeon and peer coach in this group will continue to communicate through the web-based platform. A third group will be assigned to a wait list control arm, and receive one of the two interventions later in the study.
The two video-based collaborative learning approaches will be compared to the control arm to determine whether surgical performance improves, and if one of the approaches is more effective. This study will also investigate how effectively surgeons assess their own performance after coaching. Researchers will look at changes in patient 30-day post-operative outcomes, as well as two years after surgery to see how often the hernias recur.
Dr. Greenberg’s Research Program
Dr. Greenberg’s multi-disciplinary research program is dedicated to improving the quality and safety of surgical care. Two overall goals guide her work:
1) To improve operative performance and patient safety
2) To decrease practice variation and engage patients and other stakeholders in promoting high quality surgical care for patients with cancer
A Professor of Surgery and the Morgridge Distinguished Chair in Health Services Research, Dr. Greenberg is a surgical oncologist with a clinical practice in breast cancer and a health services researcher. Her leadership roles at UW-Madison include Vice Chair for Research in the Department of Surgery, Director of the Wisconsin Surgical Outcomes Research (WiSOR) Program, Director of the Surgical Collaborative of Wisconsin, and Director of the Academy for Surgical Coaching™.
In addition to the AHRQ R01 award, Dr. Greenberg’s work has been funded by a variety of agencies, including NIH, AHRQ, and PCORI, with 9 million dollars in research grant funding. This project is one part of Dr. Greenberg’s internationally recognized surgical coaching work, which includes the recently established Academy for Surgical Coaching™. The overall profile of surgical coaching has seen significant growth in recent years, as evidenced by the inaugural Surgical Coaching Summit hosted by the Department of Surgery in June 2018.
Here at the University of Wisconsin, we’re proud to engage in research that improves surgical outcomes for patients in Madison and beyond.
Author: Dana Maya, MA